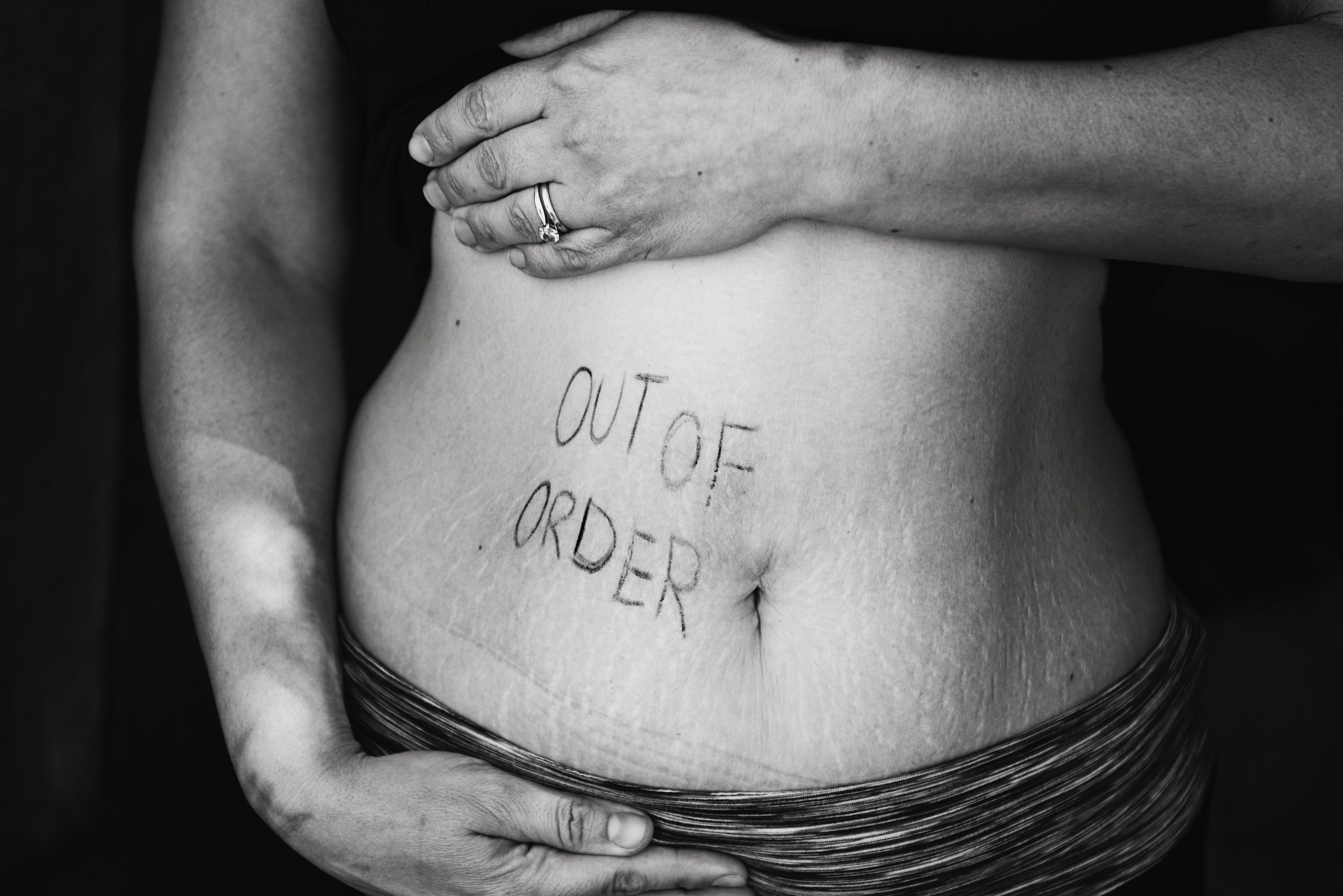
We have an epidemic of love-hate relationships with our stomachs; we love to fill them, hate their function. Not sure what I’m talking about? Take a look around the antacid section the next time you’re in the pharmacy. Or consider the number of people you know who have been prescribed proton pump inhibitors. Or maybe check the cabinet under your own bathroom sink for that family-sized canister of colorful, mild-flavored tums (which I used to eat like candy when I visited my best friend’s house in grade school- oy). That’s us, hating on our stomachs.
Let’s explore.
So we’ve chewed our food (conscientiously and thoroughly, of course) and swallowed. Our meal has traveled down the esophagus, through the pyloric sphincter, and into the stomach. Here, muscular contractions churn it with gastric juices into a partially digested, pulpy mass called chyme. After a suitable amount of digestive time has passed -generally thirty to sixty minutes- that chyme is allowed to pass in increments into the small intestine.
Digestion Phase II. Simple enough... until we find ourselves propped up on the couch with a burning weight inside our chest and the emergency tums near at hand.
Send tums plz.
Many of us are under the impression that acid in the body is bad. We’ve likely heard about the acid/alkaline diet, purchased alkaline water, and possibly cursed our own acid production for causing us GERD distress or aggravating our ulcers. In the stomach, however, high acid levels are crucial.
Gastric juices are naturally highly acidic. Aside from a few protein-specific digestive enzymes and a bit of mucosa, they’re primarily hydrochloric acid. And thank goodness! Because one of the primary roles of that high acid is to neutralize and kill potential pathogens, like foodborne bacteria. Ever wonder about that shared meal that left your partner wrapped around the toilet all night while you slept soundly a few doors down? High fives on your adequate stomach acid production (or big sympathetic hugs, if you were that partner).
Another important role of gastric juice is to begin the breakdown of protein. The digestive enzymes found in your stomach juices are protein-specific and start the process of cleaving the bonds between individual amino acids. This goes a long way towards healthful, complete digestion later in the digestive tract. So much so, in fact, that people suffering from low stomach acid can’t tolerate protein-heavy meals without discomfort, gas, pain, constipation and diarrhea.
We need stomach acid for other important digestive processes too. Many micronutrients are poorly absorbed without healthy acid levels- most notably iron, but also calcium, magnesium, zinc, copper, folic acid, beta carotene, and more. Healthy stomach acid separates these nutrients from their food source for later absorption in the small intestine.
And finally -crucially- stomach acid is needed as a signaling mechanism. As the chyme passes bit-by-bit through the pyloric sphincter and into the small intestine, the acidic contents trip a signalling pathway to the pancreas. This triggers the pancreas to realize ITS digestive juices, which include bile for fat digestion, a mother-load of digestive enzymes, and bicarbonate ions to neutralize the acidic chyme before it moves through the delicate lining of our intestines. Lower the stomach acid too much and you have a weak signal to the pancreas, resulting in less digestive enzymes and a resulting inability to digest and absorb the nutrition in your food.
Hello intestines? It’s me, acid.
Ok. So we need stomach acid. But what if we’re one of the many dealing with persistent acid reflux?
Unfortunately, the most common side effects of low stomach acid are exactly the symptoms we mistake for HIGH stomach acid. The feeling of heartburn, discomfort after meals, and burning in the esophagus can ALL be counter-intuitively caused by a stomach too alkaline. If you don’t believe me, consider this: stomach acid naturally decreases as we age, during times of stress, and over the course of a day. And it’s exactly in these scenarios that we see the highest complaints of stomach acid issues.
The process that’s happening when we experience acid reflux or GERD is a malfunction of the esophageal sphincter. This is the small valve that our food passed through as it makes its way from the mouth, through the esophagus, and into the stomach. When pressure causes that valve to open the wrong way and allows stomach contents to move north, the burn is real. Even relatively low stomach acid levels contains far, far more acid than the esophagus enjoys.
There are a variety of causes for this sphincter malfunction. It can be as simple as over-consumption, explaining that post-Thanksgiving dinner heat. It can also be caused by lying down or bending over frequently after a meal, so stay woke. But a far more concerning cause that is rarely discussed in common literature (or -sadly- the doctor’s office) is bacterial overgrowth.
The high acid of the stomach is supposed to keep bacterial colonies at bay. I love a good microbiome as much as the next person, but its place -digestively speaking- is in the large intestine. When acid levels begin to drop, it allows resilient species to begin setting up shop in our stomachs. They like it there. The food options are stellar.
As always, bacteria ferment carbohydrates extremely well. Depending on the species, fermentation can cause a lot of gas. Gas results in pressure, and when this pressure pushes against our pyloric sphincter, it can force small amounts of the stomach’s contents upwards into the esophagus. And there it is: acid reflux.
Another downside of bacterial residents is damage to the mucosal lining of our stomach. This lining is produced to protect our cells from damage caused by our ideal (high!) acid levels. Certain pathogenic species, H. pylori being a common one in stomach literature, degrade this lining. When that happens, we’re prone to pain, damage, and ulcers from acid damage. But remember, the root cause once again is low stomach acid. While we might need to temporarily lower the acid further to prevent undue pain and more tissue damage, we should never consider that a long term fix.
Whether the chicken or the egg -bacterially speaking- came first becomes inconsequential when we artificially lower our stomach acid through proton pump inhibitors and OTC bicarbonates. This sets us up for this bacterial overgrowth in the long run. We also leave ourselves vulnerable to food born pathogens, gut damage, and malabsorption over time.
Let’s put out that tiny, esophageal fire.
So what to do if we’re feeling the burn?
The first step is to reduce the highly fermentable foods in the diet. This includes carbohydrates of all types, from the sugar in maple syrup, to the starches in crackers, to the fibers in fruit (and -above all- the ridiculous, polysaccharide additives in nut milks like guar gum, carrageenan, and the like). This move reduces the food sources for any pathogenic bacteria that have moved into your stomach and often improves symptoms in short order. Most people notice differences within a week to a month, but every GI tract is its own special snowflake. That said, you don’t want to limit fruits and vegetables in all their phytochemical goodness for too long, so experiment gently with vegetable tolerance throughout. Remember that in general, cooked vegetables will be easiest to digest.
The next move is a little more ballsy: ADD acid. By helping your stomach return to its glory days of acid levels, you can lower the pH to uncomfortable levels for your bacterial frenemies and reduce the gas that causes the reflux. There are a few ways to go about this.
The gentlest trials can be done by including about 2 tablespoons of lemon juice or apple cider vinegar in about 2 ounces of water with your hearty meals. Sipping wine helps too, but I don’t advise this for three meals a day. It’s also important to avoiding drinking loads of water while you’re eating; this dilutes whatever acid you DO produce and makes it easier for pathogenic bacteria to thrive. Think about this one the next time you’re dining out, surrounded by health conscious water-guzzlers, and note that many other countries do not drop a complimentary water glass at each seat.
Digestive bitters are a beautiful, traditional tool to try at this stage too. Urban Moonshine is a favorite brand of mine (no affiliation) and their organic digestive bitters can do wonders for stimulating digestive juices and boosting our acid production.
Some people need the big acid guns, however. Disclaimer here to please work with a doctor or other health professional on this step. Also to NOT use these supplements if you’re on an NSAID regimen as these weaken the stomach lining. Hydrochloric acid is available OTC as a digestive supplement, typically sold in tablets that include pepsin, a helpful protein-digesting enzyme. They’re meant to be taken immediately before or with a meal, starting with a very low dose, and gradually increasing the dosage over a period of weeks until you feel a slight heat after ingesting them. This signals that your acid levels are (at long last!) higher than needed. At this point, you reduce the dosage to your last comfortable place and maintain this for a few months. Eventually, you wean off of these tablets in the same way you eased in. The goal is to inspire your stomach to ramp up its own production in an effort to maintain these new, healthier levels. It frequently works; HCl + pepsin supplements can be wildly life changing for people with acid reflux. They were also commonly prescribed for stomach issues until the pharmaceutical world got behind the antacid strategy.
Some benefit can also be had by including more ferments in the diet, provided you don’t suspect a candida overgrowth or other yeast issue. Adding small amounts of sauerkraut or kimchi to breakfast eggs, enjoying an organic kefir, or sipping an afternoon kombucha can all assist in restoring proper acid and stomach function.
But whatever you do, don’t -please don’t- kick the stomach acid can down the road. The long term effects on gut health further down the digestive tract are dire. It’s a hop, skip and a jump from acid suppressants to gas, bloating, diarrhea, and constipation as damage accrues in the intestinal tract. Pathogenic bacteria are allowed to flourish throughout. Nutrient absorption decreases. Other seemingly disconnected symptoms like brain fog, headaches, or skin issues follow. Inflammation rises, weight increases, and hormones shift. It might seem ridiculous to tie all of these dramatic symptoms in with a bit of stomach juice, but it’s not even a little uncommon. The stomach is the beginning of all digestive health. With every client I see dealing with seemingly lower GI issues, I always -ALWAYS- consider the stomach first.
Feeling generally healthy? GREAT! Here are three things to incorporate for your best stomach health:
Don’t drink large amounts of water with your meals, but instead hydrate between meals. Sip only as needed for comfort when you’re eating.
Include natural sources of acid with your meals when available, such as fermented foods, vinegars, lemon or lime juice, a dollop of yogurt, and acidic sippers. Luckily, you’ll notice these fit naturally with most meals and are a part of cultural food traditions.
Avoid refined foods that effectively feed pathogenic bacteria, like crackers, pastries, white bread, white rice, and more. Note that gluten-free foods are especially guilty here- they’re typically made from high levels of refined starches from potatoes, rice, and other grains or tubers.